Something you may not know about the amazing immune system is that you have two of them. Yep— innate and adaptive. I’ll explain what makes them unique…
I chose to attend University of Akron after undergrad to work on research in immunology— my thesis involved the innate immunity’s response mechanisms, so you can imagine why I find this topic fascinating.
Innate immune system
My favorite example of the innate immune system is the skin— a hugely important organ that protects all of your fragile body parts. But the skin is not the only example of your innate immunity. The innate immune system is your first line of defense and response to whatever life throws at you. Did your baby sneeze in your face? Did you accidentally pet a dog you are allergic to? Did you discover someone put peanut butter in the pie at thanksgiving and you’re reaching for the epipen? Did you eat a worm as a 4 year old? There are special protective mechanisms in place around and in your body to identify threats and attempt to neutralize them before they become a major issue. Does your innate immunity always prevent threats at a 100% success rate? No— but imagine if you had no protection like it whatsoever— scary.
Those pesky allergies!
You know how inhaling a whiff of pollen causes a sneeze and a cough and watery eyes? This is due to the innate immune cell basophil and an antibody called IgE (one of five antibody types). The basophil is one type of white blood cell. Basophils have histamine. Histamine is released from the basophil that’s hanging out in your nose lining (and eyes and throat, etc). Histamine causes the nose to run, the eyes to water, the throat to feel itchy, and other uncomfortable allergy symptoms to quickly arise. Antihistamines such as Benadryl and Claritin calm the histamine down allowing your inconvenient symptoms to subside. The pollen landed on your nose hairs (another innate immunity structure), the antibody IgE recognized this enemy pollen, and this set off an alarm to the immune cells waiting to pounce on something it doesn’t like. Your IgE antibodies (memory of that pollen allergy) and basophils sensed the enemy inhalant, and your response kicked into gear. The innate immune response is generally very quick, which is absolutely on purpose and by design.
Spotting a viral invader
So, basophils are just one relatable example of one of your innate immune cells trying to stop something from harming you. If we are talking about encountering a virus (for example, the slightly known influenza virus), there are specific innate immune white blood cells called phagocytes that perk up upon a viral particle entering the body (through the nose or the mouth, for instance). They quite literally “eat” the virus and set off a cascade of events to not only “spread the word” to other immune cells that a virus is in our midst, but to study/memorize the virus so as to fight it and neutralize the threat ASAP.
Physical barriers
The innate immune system isn’t just about the white blood cells, though. As I said, the skin is one of the most visible first line protections against the environment. Eyelashes, too, serve to protect the sensitive eye tissue. Tears exist to sweep the exposed part of the eye and clean it of foreign debris and bacteria that the air carries. The mouth is filled with protective enzymes and mechanisms to fight bacteria in the food you eat, for example. Your airway is lined with tiny hair-like cells called cilia that pulsate particles back out of the mouth to protect the lung tissue (that’s why we cough—it’s the motion of the cilia that “tickles” us). To take a deeper, nerdier dive into the physiology of coughing, I linked a cool illustrated video here: https://youtu.be/fn1XjzXQrwY
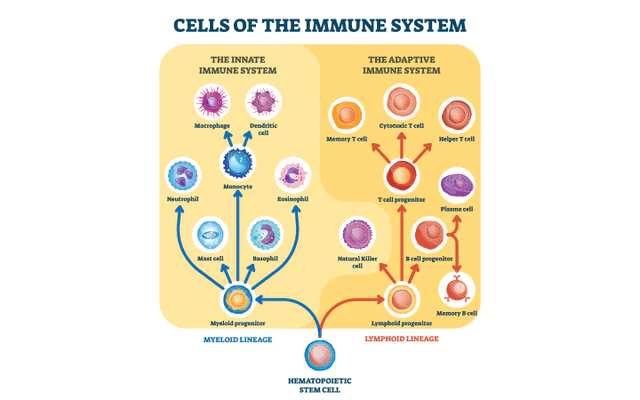
I like this infograph that details other players in the immune system…I don’t review each cell in this post for sake of brevity, so take a look if you feel like geeking out.
Thanks for the memories…
OK so your front line security guards did their jobs. Now what? Adaptive immunity gets its turn. While the innate immune system is always on, always alert, and always working, adaptive immunity is always present in the background. This arm of your immune network represents the immune system’s memory; the storage of all things learned and processed. Your innate immunity is constantly on guard and learning while your adaptive immunity is constantly remembering and applying.
Never forget…
One example of your adaptive immunity is the antibody. Antibodies are created as bits of memory when your innate immune cells fought chicken pox at age 5 (varicella zoster virus), or when they fought mononucleosis your junior year of high school (mononucleosis is caused by the Epstein Barr virus, EBV). The type of antibody that remembers that EBV infection, called IgG (another one of five antibody types), will pop up on your bloodwork 10 years after original infection. Not all memory antibodies robustly stay around like the ones after mono or chicken pox. Depending on the offending agent, a short or a long-lasting impression is left in the adaptive immune realm. The common cold is something we catch several times over a lifespan because our memory of such a virus is short-lived. Each person has their own trends in immune strength, response, and memory, but the general trend is similar per particular illness.
Below is a beautiful infograph showing each of the five antibody types. I’ve already gone over two in this post, IgE and IgG. Quick little facts about the other three: IgM is our immediate, acute phase antibody. Within an acute phase of an illness (meaning you recently contracted it), such as Hepatitis C, IgM circulates heavily in your system– think of it as the short term memory antibody that teaches the long term antibody, IgG, what’s going on and what to remember. IgA lives in the nose/ airway/ stomach for those outside substances inhaled and swallowed. You’ll also find IgA in your tears and in a mother’s first few ounces of breastmilk, called colostrum. IgD is least understood. We find it in higher amounts in newborns to around 6 months. We know that IgD is IgM’s sidekick. IgM, remember, helps identify a virus or offending agent as soon as the human body encounters it. IgD kind of helps IgM recruit other immune cells to create that long lasting memory we aim for.

Natural born killers…
My thesis in grad school focused on the natural killer T-cell which forages the blood to spot cells that look slightly “off.” These cells can look slightly different on their outer membranes, signaling, for instance, that a virus likely infected it (the virus must have gotten past those phagocytes of ours)!. NK-T cells can also spot a tumor developing. If it IDs a strange/changed cell, the NK-T cell kills it by releasing toxins onto the “strange” cell’s surface.
Autoimmunity
I cannot write about the immune system without bringing up autoimmunity. This is quite a vast and heavy topic, but I want to mention a few key takeaway points. As you know, there are numerous autoimmune disorders, and each has very specific reasons for being defined as such. A few common diseases the population is generally aware of are rheumatoid arthritis, lupus, multiple sclerosis, and celiac disease. In each of these diseases, the body’s normal line of defense is altered in some way; it’s programmed to attack your own human body tissues rather than defend it.
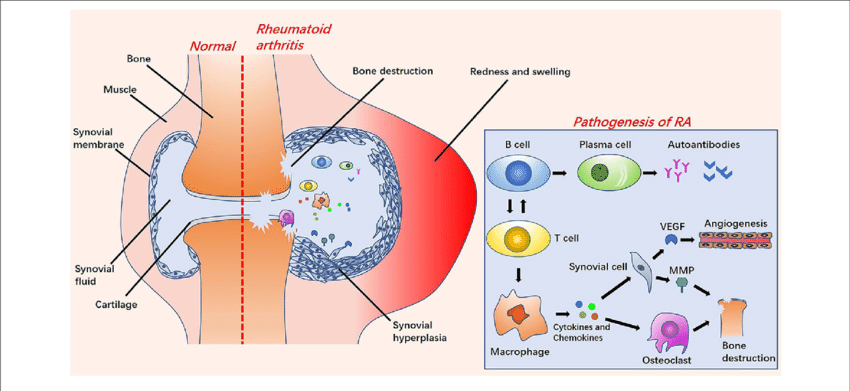
Rheumatoid arthritis involves the immune system thinking joints in the body are foreign and should be attacked. There is something called rheumatoid factor, which binds to the antibody IgG. This bound unit attacks the joint linings, and their unfortunate goal is to destroy the collagen and cartilage in those spaces. The smoothness of that joint’s motion is reduced by this process. Swelling, tenderness, stiffness, and pain occur as a result. Picture a bunch of antibodies clogging the tiny space between your knuckles, or the knee joints, or the toes. There is so much inflammation over time that deformities arise in these areas. Fingers/hands begin to angle in different directions (termed a ‘swan neck deformity”), and the knuckles look enlarged. Folks with RA whose feet are targeted sometimes become unable to walk due to the toes and bones becoming so diseased. This is all because the immune system decided it didn’t like these joint tissues. As a primary care provider, I feel one of the most tortuous and painful diseases I see regularly is RA. See the helpful graphic below.
Back to basics
One hot topic of wellness in our culture is the immune system: how to boost it, how to support it, and how to avoid harming it. The immune system is a natural, complex, and beautiful mechanism in place meant to keep us alive. It’s a primal line of defense that really requires only a few things to remain well-functioning: adequate nutrients in the form of food, hydration in the form of water, of course, and rest in the form of adequate and quality sleep. While many feel that supplements are the answer, especially in our “quick-fix” society, your best bet is truly to focus on the aforementioned basics (but if you have an actual deficiency in something, of course you should correct it). And while taking zinc and vitamin C is certainly fine, it’s not going to be your main saving grace. It sounds cliche to state that reducing stress is also imperative to maintaining a strong immune system–cliche, but very very true. The more the human body exists in survival mode, in anxious states of mind, and in overworked capacities, it will age quicker and result in a tired system.
Since early 2020, the human immune system has been widely discussed around the world more than I can ever remember (pandemic anyone?), and I found myself answering countless questions from my family, friends, and patients regarding how our bodies work in this regard (especially when the COVID vaccine came around). This inspired me to detail this part of human anatomy/physiology. I hope that you close this page with a better understanding of our crucial and amazing immune system. After all, you have it to thank for being alive.
References
Britannica. Antibody biochemistry. Retrieved 10 March 2023 from: https://www.britannica.com/science/antibody/Antibody-structure-and-classes
Britannica. Rheumatoid arthritis. Retrieved 11 March 2023 from: https://www.britannica.com/science/immune-system-disorder/Autoimmune-diseases-of-the-thyroid-gland#ref719068