No exaggeration, one of the most commonly undiagnosed and untreated conditions I see is sleep apnea. I officially recommend a sleep study to at least one patient per day. We all know someone who has sleep apnea. We all know someone who wears the mask to sleep at night, and we may all know someone who SHOULD wear theirs and they refuse to do so (those people hear my wrath of warnings when they admit this to me). I think it’s also safe to say we know someone who needs a sleep study but refuses to get one. OK, so…YOU reading this— you seriously could have this disorder. Let’s screen you the way that I screen my patients…
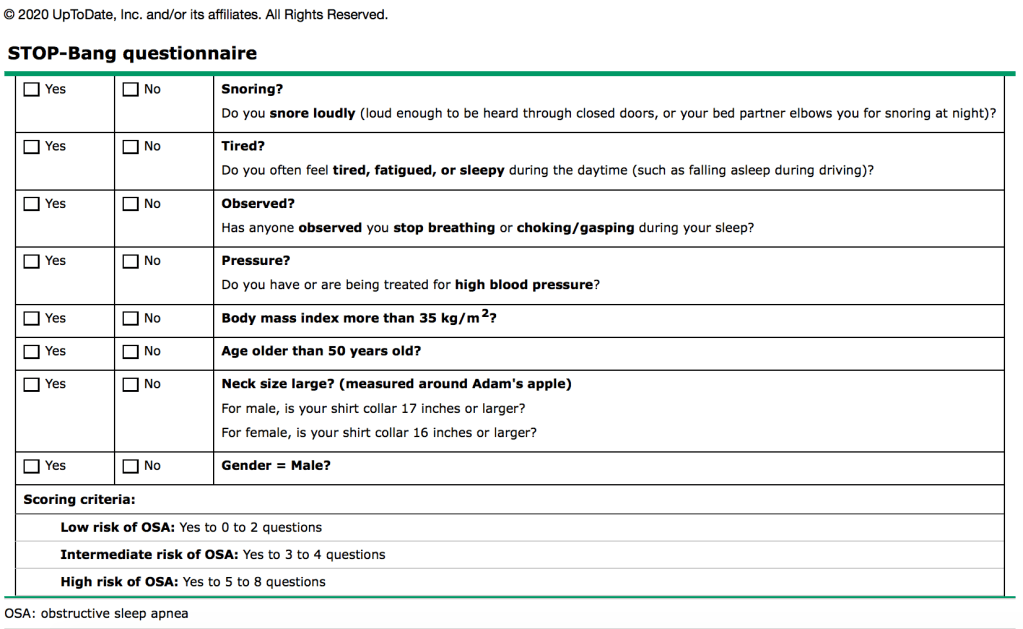
This is the STOP-BANG assessment (below). It’s a tool I use to stratify someone’s risk for obstructive sleep apnea (OSA). It’s out of 8 points. Now, may I say that this assessment of course is not perfect and scoring a 7 or 8 does not mean you for sure have OSA. However, it would be worth a chat with a sleep specialist. There is no perfect screening tool for OSA—there are several of them. The real test is THE test. The overnight sleep study AKA polysomnography.
I’m sure you’ve heard negative remarks and dramatized horror stories about a sleep study. You look like Medusa with lots of wires stuck to your head (they monitor brain activity during sleep), and the adhesive sticks in your hair, and the bed isn’t comfortable, and yada yada yada. I hear these same remarks from patients when I tell them they need to get a sleep study. They give me 30 reasons why they don’t want to….but I give them one reason to go through with it: people die in their sleep from untreated sleep apnea. Don’t let that be you. The adhesive will wash out of your hair, don’t worry.
Let’s back up and talk about what sleep apnea really means. There are two kinds of sleep apnea, obstructive and central. Obstructive is more common and the one mainly discussed in this post. Central is basically when the brain doesn’t tell the body to breathe because it’s not communicating efficiently with the lungs/chest wall muscles (most commonly seen in heart failure or stroke patients and those who use opioids). Obstructive is when the actual airway is anatomically altered somehow to not be favorable in getting airflow through. This is why your neck circumference matters and your BMI matters during your risk assessment. OSA is defined as “recurrent obstruction of the pharyngeal airway during sleep, with resultant hypoxia and sleep fragmentation” (UpToDate, 2020). The upper airway (your throat area) narrows, and the air passing through becomes turbulent. The soft palate of the mouth flutters, causing audible snoring. That’s why you can hear Grandpa snoring all the way down the hall. OSA happens when the upper airway completely collapses on and off throughout the night (or a catnap!) With this, inadequate oxygen is getting to your body’s organs (heart, brain…you know, the important ones) and you’re left with daytime fatigue or the feeling that you barely slept a wink after 8 hours.
Seriously, though, think for a minute about your risk. You may have mental fog to the point that you think you’re getting dementia. You may be very moody. You may awaken each morning with headaches and a dry mouth. You are tempted to fall asleep while driving (maybe you have done this at a red light). You can’t sit on the couch without nodding off. You wake yourself up snoring or gasping for air. None of this is healthy, and you should consult with a sleep specialist. I keep our local specialists busy with referrals. I do NOT fool around with missing OSA. Despite my crusade on catching OSA, it’s estimated by the American Sleep Apnea Association that 80% of moderate-severe OSA patients in America are undiagnosed. About 22 million Americans have sleep apnea, and the number is growing.
Sometimes your insurance will dictate what kind of sleep study you can do—most sleep overnight at a sleep lab, whereas some have to do an in-home test. But I will say, the in-home is not preferred for many reasons. As a provider, I want to know that you’re hooked up correctly, a professional is watching your live recordings, and that you complete the study in full. The home studies may not pick up cases of mild sleep apnea, so unless insurance or some other unique situation calls for the in-home, you’re going to be sleeping at the lab. And even if you do the in-home, you often have to repeat the study in the lab, anyway. Just opt for the lab from day 1.
While you are sleeping at the lab during your test, they look for many things. They record your limb movements. They look at how many times you wake up and why. They watch your oxygen levels at all times, especially how many times you dip below 88% (oxygen not getting into the blood stream very well). They really watch how many times you stop breathing. That last one scares people the most. Sometimes it’s 5 times per hour (mild OSA) and sometimes it’s over 30 (severe OSA). Yes, you read that right. When you stop breathing, sometimes it’s for 10 seconds straight, and your reflexes kick in to jolt you awake to breathe. People do this multiple times an hour, which leads to non-restorative, restless sleep. When you stop breathing for several seconds, the stress hormone cortisol releases into the blood stream, stressing the heart and metabolism, and spiking blood sugar levels. This is why those with untreated sleep apnea have stronger risks of developing heart disease and diabetes.
OK so what if your test shows you have OSA? You’ll return for a second sleep study shortly after, but this time it’ll be with a machine. The machine will allow continuous positive airway pressure (CPAP) into your airway via a face mask, and boy, will you notice a difference! The technicians will decide at which level to dial your machine for suitable sleep at home. Patients who are compliant with their sleep machine tell me they can’t imagine sleeping without it because they feel so much better in the mornings compared to before. Some wait 5, 10, even 15 years before they do the study. Most go through with it to appease their spouses. Hey, I don’t care how we get you there, just get there! Insurance usually covers your machine, but many carriers monitor how many hours you use it. If you don’t use it at least 4 hours per day, they’ll make you buy it to keep it. Just use it— you’ll be better off doing so!
If you’ve been diagnosed with OSA, you’ve probably heard “if you lose weight, you won’t need that machine anymore!” Well, maybe/maybe not. The reason that weight loss works to eliminate OSA in some folks is that increased fatty tissue in the neck/facial structures causes the airway to narrow and be literally weighed down. But if you’re of healthy weight already, weight loss won’t help your case. Your airway is naturally prone to collapse during sleep for other reasons such as bone structure or tonsil/uvula/tongue size, and your OSA will be a lifelong diagnosis. There exists a surgical procedure called the Uvulopalatopharyngoplasty (I know you didn’t try to sound that one out after Uvulop-). It’s also called UP3. It’s where a surgeon remodels the throat by removing the uvula, the tonsils, adenoids, and any excess tissue that cause airway narrowing. I saw this in my ENT rotation and it allowed a man to avoid using a nightly CPAP. It doesn’t always prevent the use of a CPAP but some people get the surgery with those hopes. There is also a “mandibular advancement device” that pushes the jaw forward if that is your suspected problem. Overall, your sleep specialist will recommend the treatment plan best for you.
Breathing is necessary for life, right? So is good sleep. Sleeping is when the body relaxes, restores, and refreshes. It’s when healing occurs. During sleep, your brain takes a look at everything you encountered that day from street signs to people’s faces to the 10 news articles you read and decides which is worth making a memory of and which is unimportant. The less you sleep well, the less your brain will retain. Poor sleep matched with poor breathing is a recipe for disaster—and poor quality of life. If your spouse or family has been hounding you to get a sleep study, they likely have a good reason. Set your pride aside and talk to a specialist. Sleep is one of my most discussed subjects with patients, and we are finding sleep apnea is often the underlying cause to numerous complaints and conditions.
I hope you feel more informed about OSA and understand where you fall in the risk of having it. Sleep tight.
References
American Sleep Apnea Association. Sleep apnea information for clinicians. 2020. Retrieved from https://www.sleepapnea.org/learn/sleep-apnea-information-clinicians/
Johns Hopkins Medicine. The dangers of uncontrolled sleep apnea. 2020. Retrieved from https://www.hopkinsmedicine.org/health/wellness-and-prevention/the-dangers-of-uncontrolled-sleep-apnea.
UpToDate. Central sleep apnea: Risk factors, clinical presentation, and diagnosis. 2020 January. Retrieved from https://www.uptodate.com/contents/central-sleep-apnea-risk-factors-clinical-presentation-and-diagnosis?search=central%20sleep%20apnea&source=search_result&selectedTitle=1~141&usage_type=default&display_rank=1.
UpToDate. Clinical presentation and diagnosis of obstructive sleep apnea in adults. 2020 January. Retrieved from https://www.uptodate.com/contents/clinical-presentation-and-diagnosis-of-obstructive-sleep-apnea-in-adults?search=stop%20bang§ionRank=1&usage_type=default&anchor=H719630181&source=machineLearning&selectedTitle=2~13&display_rank=2#H1595203612.
UpToDate. Pathophysiology of obstructive sleep apnea is adults. 2020 January. Retrieved from https://www.uptodate.com/contents/pathophysiology-of-obstructive-sleep-apnea-in-adults?search=osa&source=search_result&selectedTitle=5~150&usage_type=default&display_rank=5.
