Constant pain. Tenderness. Fatigue. Merely sitting still hurts. This is fibromyalgia. Around 2% of Americans suffer from this chronic pain disorder (10-ish million), but I personally have a feeling this is an underestimate. I see this at least weekly at work. To be frank, some clinicians doubt its existence. Why? Because there is no absolute definitive test for such a diagnosis. The testing is subjective— pain is subjective, so we rely on the patient to make that final affirmation. It usually takes years for a patient to get their diagnosis because they find it hard to be taken seriously. I know a fibromyalgia person when I see one— their skin is tender and sometimes just grazing over a specific body site brings tears to their eyes. They look exhausted, downtrodden, and have tried pretty much everything for pain relief. They’re usually a 30 to 40-something female, but all ages can be victim to FM.
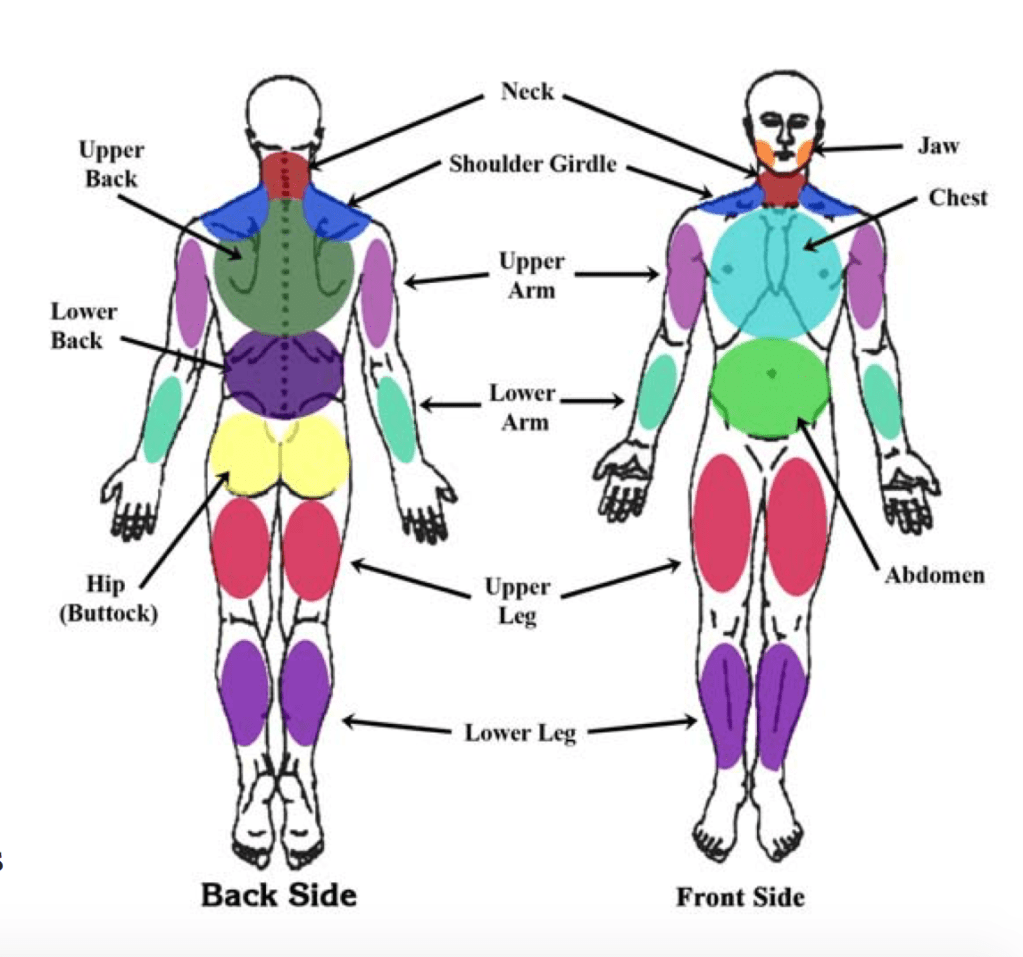
Fibromyalgia is called a diagnosis of exclusion. We rule out other causes using diagnostic tools such as x-rays, MRIs, CT scans, and blood work. We look for arthritis in associated joints, disc abnormalities of the spine, nerve impingements, rheumatoid arthritis, lupus, and muscle strains, to name a few. And honestly, a rheumatologist usually helps to give the final diagnosis, if not a pain specialist, or us folks in primary care. If everything looks uneventful on testing, we do a specific physical exam to see where you’re experiencing pain and tenderness. There are defined points of tenderness in someone who we think has fibromyalgia (diagram below). If the patient is tender AND experiences resting pain in 11 of these places, and we cannot figure out any other cause for their pain, we label it fibromyalgia. The definition of FM is widespread pain in all 4 quadrants of the body for at least 3 months, accompanied by abnormal pain perception processing.
Someone with FM is more sensitive to pain than the average Jane. People with fibromyalgia will tell you that their pain fluctuates. Sometimes the weather can worsen it (hint: cold), but usually if the patient has a depressive episode or is sad or anxious, the pain intensifies. This is a testament to how mental health has very physical manifestations. FM patients don’t sleep well, partly because they cannot find a comfortable state to rest. Ironically, quality sleep helps FM to reduce in intensity. Figures.
The condition is much more common in women (different sources say anywhere from twice to 10 times more common). Why? Who knows. We say “who knows” a lot about FM. There is no specific gene that causes it. There is no specific heredity pattern, though we do see trends in families. There are whispers about a blood test to diagnose fibromyalgia, but it’s not available yet. Don’t run and ask your doctor for a fibromyalgia blood test because I hinted it exists, because it doesn’t. Don’t get me in trouble. But I will tell you this: scientists at THE Ohio State University have found promising leads into this particular blood test. Fifty FM patients provided blood samples, which were then compared to blood of patients with rheumatoid arthritis, osteoarthritis, and lupus. Distinct differences in molecular patterns were observed in FM blood. These researchers aim to have the test available in 5 years (2024). They’d first like to try this method on a larger sample size prior to public availability. I think that’s a great idea– better be safe than sorry. Man, those Buckeyes really do dominate on the field and in the classroom.
You can treat fibromyalgia in many ways, but nothing will likely ever make your pain completely resolve. The pain is sort of a part of your norm, but you can control it somewhat. Physical therapy, staying physically active and fit, managing stressors/depression/anxiety, participating in cognitive behavioral therapy, and simply educating yourself on the disease helps. There are oral medications that have been proven to reduce FM pain—anywhere from antidepressants to anti-inflammatories to certain stronger pain medications. Opiates are NOT indicated for the treatment of fibromyalgia because man, is that a slippery slope! You’ll notice you’ll depend on them, and being that opiates are highly addictive in many people, don’t even go there. Oh, and it’s imperative to stay hydrated (I mean pure water, not soda or tea) and try to get plenty of quality sleep every night.
One fascinating study looked at personality traits of those with fibromyalgia. The results showed that out of 48 FM women, those who reported the highest pain levels were also highly neurotic and displayed impulsive behaviors (Boucourt et al, 2017). This is correlation, not causation—however, the link is interesting.
Another study by the same primary author (Boucourt, 2019) reviewed comparisons between FM and other disorders such as rheumatoid arthritis and spondyloarthritis. The conclusion was this: “Compared with other rheumatic diseases, fibromyalgia has a greater impact on daily life; patients have more difficulty adjusting to the disease and generally use poorer strategies to cope with pain.” This is where I come in. It is my responsibility in primary care to teach FM sufferers on how they can manage their pain, ensure they recognize their triggers, and offer any support I can to keep their body healthy and their spirits up. I can treat their associated mood disorder(s), refer for physical therapy, set them up with my in-office counselor, and prescribe safe but effective medications for pain. They can also get regular massages (if not on a terribly tender day) and practice yoga or self-guided stretching.
So do you think you may have fibromyalgia? Go to this site for an extensive questionnaire. It’s nicely comprehensive. This is a tool to screen yourself, but to also take to your provider to confirm your suspicion. (https://neuro.memorialhermann.org/uploadedFiles/_Library_Files/MNII/NewFibroCriteriaSurvey.pdf).
Another nice source is https://fibroandpain.org/fm-fact-sheet-2. I linked you to a fact sheet so that you can briefly understand what FM encompasses and if it sounds like your symptoms. Click around the website for more information.
Quality of life is EVERYTHING. Our number of years is not guaranteed, but what we do know is how we feel from day to day. If you feel physically and/or mentally miserable and feel helpless with these struggles, please reach out to someone you trust in the medical community. We are here to help guide you to answers. If your answer is a diagnosis of fibromyalgia, professionals are ready to provide tools and therapies to assist you in getting that quality of life back—to not being someone controlled by fibromyalgia, but to being someone who happens to have it and who lives each day defeating it.
References:
Boucourt E et al. A Comparative Study of Fibromyalgia, Rheumatoid Arthritis, Spondyloarthritis, and Sjögren’s Syndrome; Impact of the Disease on Quality of Life, Psychological Adjustment, and Use of Coping Strategies. Pan Med. 2019 Nov 9. E-published.
Boucourt E et al. Comparison of the Big Five personality traits in fibromyalgia and other rheumatic diseases. Joint Bone Spine. 2017 Mar;84(2):203-207.
CDC. Fibromyalgia. Retrieved November 17, 2019 from https://www.cdc.gov/arthritis/basics/fibromyalgia.htm.
Fibromyalgia Network. New Clinical Fibromyalgia Diagnostic Criteria. Retrieved November 17, 2019 from https://neuro.memorialhermann.org/uploadedFiles/_Library_Files/MNII/NewFibroCriteriaSurvey.pdf.
NFMCPA. Fibromyalgia. Retrieved November 17, 2019 from https://fibroandpain.org/fibromyalgias
Sandoiu A. Groundbreaking blood test detects fibromyalgia. 18 March 2019. Medical News Today. Retrieved November 17, 2019 from https://www.medicalnewstoday.com/articles/324735.php#1
